Pregnancy and Fetal Cells: New Actors in Wound Healing
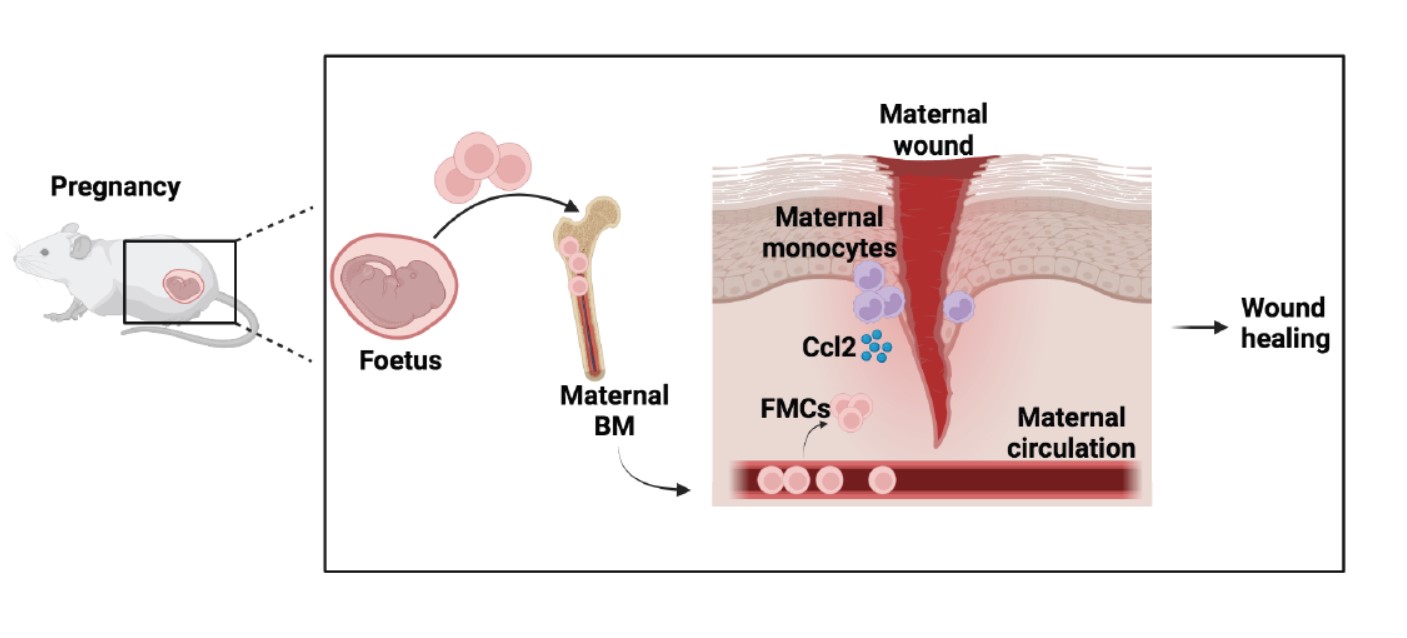
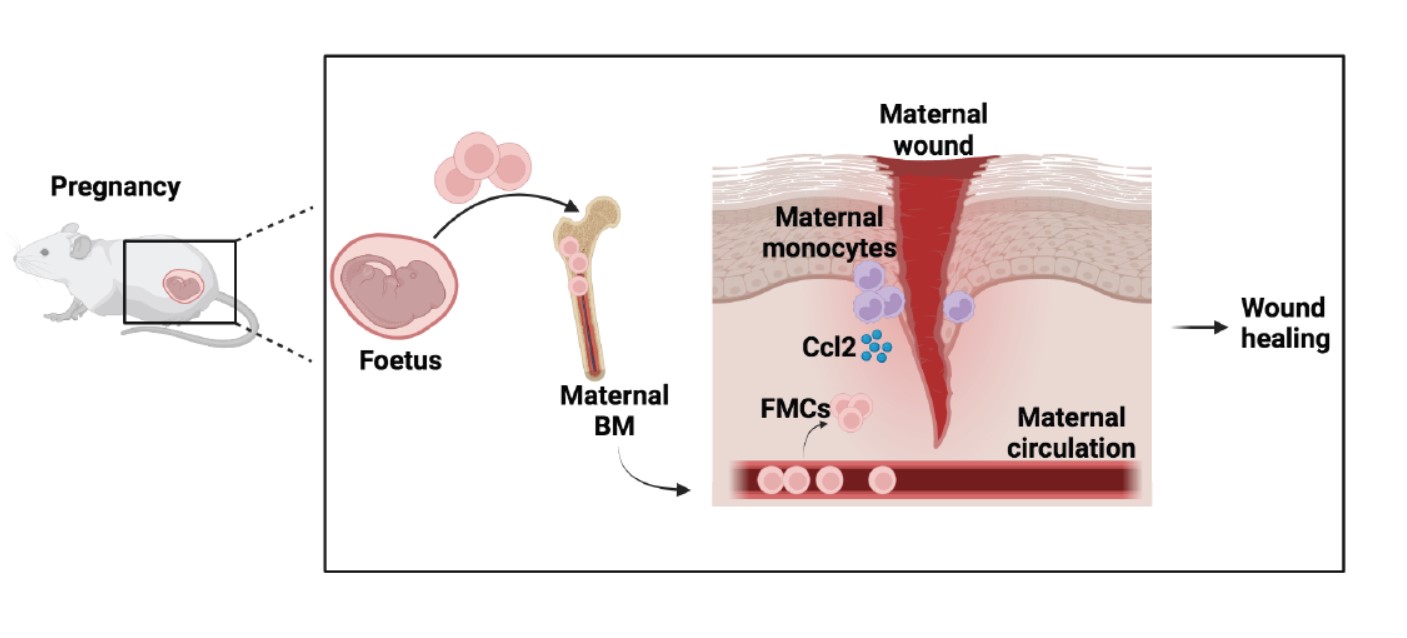
Wound healing is a complex biological process that involves various tissue structures and cells, both local and distant. One significant factor in this process is the presence of fetal microchimeric cells (FMCs) that enter the maternal circulation during pregnancy. These cells not only engraft into different organs but also nest in the maternal bone marrow (BM). Interestingly, FMCs are well-tolerated by the immune system and can persist for extended periods, potentially throughout the mother’s lifespan.
In the case of maternal injury, FMCs actively contribute to wound healing by migrating to the damaged tissue and adopting the phenotype of the affected organ. Recent research by Castela et al. discovered that during the initial stage of skin wound healing in pregnant mice, there is an increase in the production of a chemokine called Ccl2. Monocytes and endothelial cells produce this chemokine, which in turn induces the recruitment of FMCs through Ccr2 signaling. FMCs express high levels of the Ccr2 receptor, making them responsive to Ccl2. The injection of Ccl2 further enhances wound healing by promoting neovascularization, a process critical for tissue repair. Interestingly, these injections had no effect on wound healing in virgin mice, highlighting the essential role of FMCs and their interaction with Ccl2 in promoting maternal angiogenesis and wound healing.
Wound-healing disorders can affect adult females years after delivery. Since fetal cells persist in the maternal bone marrow throughout life, researchers investigated the effects of Ccl2 in a delayed wound-healing model during the early and late postpartum periods. Using mice that had given birth, the authors treated them daily with a topical application of clobetasol cream, which induces skin atrophy and delayed wound healing, followed by excisional skin wounds on the lower back. Ccl2 was injected into the wounds on specific days after wounding. The treated mice showed improved wound closure kinetics, increased proliferation of epidermal and dermal cells, and enhanced neoangiogenesis (formation of new blood vessels). Thus, Ccl2 recruitment of FMCs improved delayed wound healing in the early and late postpartum periods in mice.
In line with this research, Alkobtawi et al. found that FMCs also play a crucial role in healing leg ulcers, a significant complication of sickle cell disease (SCD). SCD is a prevalent genetic disease worldwide, characterized by long-lasting, recurrent, and challenging-to-treat ulcers. These ulcers cause severe disabilities and significantly impact patients’ quality of life. By comparing multiple blood parameters of a cohort of SCD patients, the authors discovered that SCD women who had given birth experienced a lower burden of leg ulcers compared to nulliparous women.
These studies provide new insights into fetal stem cell therapy and suggest that pregnancy improves wound healing in both mice and women with SCD. The higher expression of the Ccr2 receptor on FMCs enables these cells to rescue delayed wound repair in parous mice, and this advantage persists for a prolonged period after delivery. Considering the immune system’s tolerance towards FMCs, these findings also shed light on the potential use of induced pluripotent stem cells, embryonic stem cells, or allogeneic cell therapies in regenerative medicine.
Contribution of Elise Abboud, PhD, Institut Cochin, INSERM U1016, Paris.
References :
- Castela M, et al. Ccl2/Ccr2 signalling recruits a distinct fetal microchimeric population that rescues delayed maternal wound healing. Nat Commun. 2017 May 18;8:15463. doi: 10.1038/ncomms15463.
- Alkobtawi M, et al. Contribution of fetal microchimeric cells to maternal wound healing in sickle cell ulcers. Haematologica 2022;108(7):1920-1933; https://doi.org/10.3324/haematol.2022.281140.
